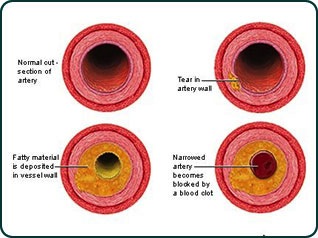
Coronary artery disease occurs when a substance called plaque builds up in the arteries that supply blood to the heart (called coronary arteries). Plaque is made up of cholesterol deposits, which can accumulate in your arteries. When this happens, your arteries can narrow over time. This process is called atherosclerosis.
Plaque buildup can cause angina, the most common symptom of CAD. This condition causes chest pain or discomfort because the heart muscle doesn’t get enough blood. Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way that it should. An irregular heartbeat, or arrhythmia, can also develop.
For some people, the first sign of CAD is a heart attack. A heart attack occurs when plaque totally blocks an artery carrying blood to the heart. It also can happen if a plaque deposit breaks off and clots a coronary artery.
Plaque buildup can cause angina, the most common symptom of CAD. This condition causes chest pain or discomfort because the heart muscle doesn’t get enough blood. Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way that it should. An irregular heartbeat, or arrhythmia, can also develop.
For some people, the first sign of CAD is a heart attack. A heart attack occurs when plaque totally blocks an artery carrying blood to the heart. It also can happen if a plaque deposit breaks off and clots a coronary artery.
Important Tests
Doctors can determine your risk for CAD by checking your blood pressure, cholesterol, and blood glucose, and by finding out more about your family’s history of heart disease. If you’re at high risk or already have symptoms, your doctor can perform several tests to diagnose CAD including—ECD or EKG (electrocardiogram)
Echocardiogram
Exercise stress test
Chest X-ray
Cardiac Catheterization
Coronary angiogram
Echocardiogram
Exercise stress test
Chest X-ray
Cardiac Catheterization
Coronary angiogram
Measures the electrical activity, rate, and regularity of your heartbeat.
Uses ultrasound to create a picture of the heart.
Measures your heart rate while you walk on a treadmill. This helps to determine how well your heart is working when it has to pump more blood.
Creates a picture of the heart, lungs, and other organs in the chest.
Checks the inside of your arteries for blockage by threading a thin, flexible tube through an artery in the groin, arm, or neck to reach the coronary artery. Can measure blood pressure and flow in the heart’s chambers, collect blood samples from the heart, or inject dye into the coronary arteries.
Monitors blockage and flow of blood through the heart. Uses X-rays to detect dye injected via cardiac catheterization.
Creates a picture of the heart, lungs, and other organs in the chest.
Checks the inside of your arteries for blockage by threading a thin, flexible tube through an artery in the groin, arm, or neck to reach the coronary artery. Can measure blood pressure and flow in the heart’s chambers, collect blood samples from the heart, or inject dye into the coronary arteries.
Monitors blockage and flow of blood through the heart. Uses X-rays to detect dye injected via cardiac catheterization.

Treatment
If you have CAD, there are steps you can take to lower your risk for having a heart attack or worsening heart disease. Your doctor may recommend lifestyle changes such as eating a healthier diet, exercising, and not smoking.
Medications may also be necessary. Medicines can treat CAD risk factors such as high cholesterol, high blood pressure, an irregular heartbeat, and low blood flow. In some cases, more advanced treatments and surgical procedures can help restore blood flow to the heart.
Content Source:Content Source: http://www.cdc.gov/heartdisease/coronary_ad.htm
If you have CAD, there are steps you can take to lower your risk for having a heart attack or worsening heart disease. Your doctor may recommend lifestyle changes such as eating a healthier diet, exercising, and not smoking.
Medications may also be necessary. Medicines can treat CAD risk factors such as high cholesterol, high blood pressure, an irregular heartbeat, and low blood flow. In some cases, more advanced treatments and surgical procedures can help restore blood flow to the heart.
Content Source:Content Source: http://www.cdc.gov/heartdisease/coronary_ad.htm
Cardiac Specialty Care
• Structural Heart Disease
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• Coronary Intervention
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Peripheral Angioplasty
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Rhythm Management
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
