Syncope (pronounced “sin ko pea”) is the brief loss of consciousness and posture caused by a temporary decrease in blood flow to the brain. Syncope may be associated with a sudden fall in blood pressure, a decrease in heart rate or changes in blood volume or distribution. The person usually regains consciousness and becomes alert right away, but may experience a brief period of confusion.
Syncope is often the result of an underlying medical condition that could be related to your heart, nervous system or blood flow to the brain.
What are the symptoms of syncope?
The most common symptoms of syncope include:
Most common causes
“Blacking out”
Light-headedness
Falling for no reason
Dizziness
Drowsiness
Grogginess
Feeling unsteady or weak when standing
The most common symptoms of syncope include:
Most common causes
“Blacking out”
Light-headedness
Falling for no reason
Dizziness
Drowsiness
Grogginess
Feeling unsteady or weak when standing
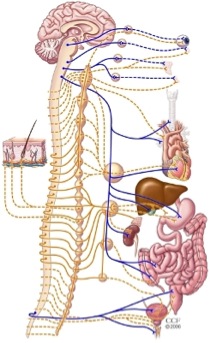
The ANS automatically controls many functions of the body such as breathing, blood pressure, heart rate and bladder. In most situations, we are unaware of the workings of the ANS because it functions in an involuntary, reflexive manner.
Syncope is often preceded by other symptoms (called premonitory symptoms), such as light-headedness, nausea and palpitations (irregular heartbeats that feel like “fluttering” in the chest).
Many people with syncope learn, on their own, to avoid a syncopal event or “passing out.” They recognize the premonitory symptoms and sit or lie down quickly and elevate their legs.
Because syncope could be the sign of a more serious condition, it is important to seek treatment right away after a syncope episode occurs.
With accurate diagnosis and appropriate treatment, syncope can be resolved in most patients.
What causes syncope?
There are many causes of syncope. If blood does not circulate properly, or the autonomic nervous system does not work the way it should, changes in blood pressure and heart rate can cause fainting. Metabolic abnormalities and anemia may also cause syncope.
The ANS automatically controls many functions of the body such as breathing, blood pressure, heart rate and bladder. In most situations, we are unaware of the workings of the ANS because it functions in an involuntary, reflexive manner.
Types of Syncope
Vasovagal syncope (also called cardio-neurogenic syncope)
Vasovagal syncope is the most common type of syncope that occurs when the blood pressure drops suddenly, reducing blood flow to the brain. When you stand up, gravity causes blood to settle in the lower part of your body, below the level of the diaphragm. In response, the heart and autonomic nervous system (ANS) react to maintain your blood pressure.
Vasovagal syncope may occur in patients who have a condition called orthostatic hypotension. In this condition, the blood vessels do not constrict normally when the patient stands, causing blood to pool in the legs and the blood pressure to drop quickly.
Situational syncope
Situational syncope is a type of vasovagal syncope that occurs only during particular situations that cause unusual patterns of stimulation to certain nerves. The “stimulus” that triggers an exaggerated neurological reflex can be a wide range of different events such as dehydration, intense emotional stress, anxiety, fear, pain, hunger or use of alcohol or drugs. Hyperventilation (breathing in too much oxygen and getting rid of too much carbon dioxide too quickly) associated with panic or anxiety also can cause syncope. Other stimuli include coughing forcefully, turning the neck or wearing a tight collar (carotid sinus hypersensitivity), or urinating (miturition syncope).
Postural syncope (also called postural hypotension)
Postural syncope occurs when the blood pressure drops suddenly due to a quick change in position, such as from lying down to standing. Postural syncope can be related to certain medications or dehydration.
Cardiac syncope
Cardiac syncope is the loss of consciousness due to a heart or blood vessel condition that interferes with blood flow to the brain. These conditions may include an abnormal heart rhythm (arrhythmia), obstructed blood flow in the heart or blood vessels, valve disease, aortic stenosis, blood clot, or heart failure.
Neurologic syncope
Neurologic syncope is the loss of consciousness due to a neurological condition such as seizure, stroke, transient ischemic attack (TIA) or other rare causes including migraines and normal pressure hydrocephalus.
In about one-third of cases, the cause of syncope is unknown.
How common is syncope?
Syncope is a common condition, affecting 3 percent of men and 3.5 percent of women at some point in life. It becomes more prevalent with advancing age, occurring in as many as 6 percent of people over age 75. Syncope affects patients of all ages, both with and without other medical conditions.
How is syncope diagnosed?
All patients with syncope should be evaluated by a doctor. Your primary care physician can provide a referral to the Center for Syncope and Autonomic Disorders for a complete evaluation to determine the cause of your syncope.
The Center for Syncope and Autonomic Disorders combines experience, expertise and a team approach to diagnosing syncope. There are several tests that can be performed to find the underlying cause of syncope. The initial evaluation includes a screening tilt table test, blood volume determination, hemodynamic testing and autonomic nervous system testing.
The syncope evaluation begins with a careful review of your medical history and a physical exam. The doctor will ask you detailed questions about your symptoms and syncope episodes, including whether you have any premonitory symptoms and the circumstances in which your symptoms occur.
Your heart rate and blood pressure will be measured and recorded while you are in different positions including lying down, sitting and standing.
Tests to determine causes of syncope
Many people with syncope learn, on their own, to avoid a syncopal event or “passing out.” They recognize the premonitory symptoms and sit or lie down quickly and elevate their legs.
Because syncope could be the sign of a more serious condition, it is important to seek treatment right away after a syncope episode occurs.
With accurate diagnosis and appropriate treatment, syncope can be resolved in most patients.
What causes syncope?
There are many causes of syncope. If blood does not circulate properly, or the autonomic nervous system does not work the way it should, changes in blood pressure and heart rate can cause fainting. Metabolic abnormalities and anemia may also cause syncope.
The ANS automatically controls many functions of the body such as breathing, blood pressure, heart rate and bladder. In most situations, we are unaware of the workings of the ANS because it functions in an involuntary, reflexive manner.
Types of Syncope
Vasovagal syncope (also called cardio-neurogenic syncope)
Vasovagal syncope is the most common type of syncope that occurs when the blood pressure drops suddenly, reducing blood flow to the brain. When you stand up, gravity causes blood to settle in the lower part of your body, below the level of the diaphragm. In response, the heart and autonomic nervous system (ANS) react to maintain your blood pressure.
Vasovagal syncope may occur in patients who have a condition called orthostatic hypotension. In this condition, the blood vessels do not constrict normally when the patient stands, causing blood to pool in the legs and the blood pressure to drop quickly.
Situational syncope
Situational syncope is a type of vasovagal syncope that occurs only during particular situations that cause unusual patterns of stimulation to certain nerves. The “stimulus” that triggers an exaggerated neurological reflex can be a wide range of different events such as dehydration, intense emotional stress, anxiety, fear, pain, hunger or use of alcohol or drugs. Hyperventilation (breathing in too much oxygen and getting rid of too much carbon dioxide too quickly) associated with panic or anxiety also can cause syncope. Other stimuli include coughing forcefully, turning the neck or wearing a tight collar (carotid sinus hypersensitivity), or urinating (miturition syncope).
Postural syncope (also called postural hypotension)
Postural syncope occurs when the blood pressure drops suddenly due to a quick change in position, such as from lying down to standing. Postural syncope can be related to certain medications or dehydration.
Cardiac syncope
Cardiac syncope is the loss of consciousness due to a heart or blood vessel condition that interferes with blood flow to the brain. These conditions may include an abnormal heart rhythm (arrhythmia), obstructed blood flow in the heart or blood vessels, valve disease, aortic stenosis, blood clot, or heart failure.
Neurologic syncope
Neurologic syncope is the loss of consciousness due to a neurological condition such as seizure, stroke, transient ischemic attack (TIA) or other rare causes including migraines and normal pressure hydrocephalus.
In about one-third of cases, the cause of syncope is unknown.
How common is syncope?
Syncope is a common condition, affecting 3 percent of men and 3.5 percent of women at some point in life. It becomes more prevalent with advancing age, occurring in as many as 6 percent of people over age 75. Syncope affects patients of all ages, both with and without other medical conditions.
How is syncope diagnosed?
All patients with syncope should be evaluated by a doctor. Your primary care physician can provide a referral to the Center for Syncope and Autonomic Disorders for a complete evaluation to determine the cause of your syncope.
The Center for Syncope and Autonomic Disorders combines experience, expertise and a team approach to diagnosing syncope. There are several tests that can be performed to find the underlying cause of syncope. The initial evaluation includes a screening tilt table test, blood volume determination, hemodynamic testing and autonomic nervous system testing.
The syncope evaluation begins with a careful review of your medical history and a physical exam. The doctor will ask you detailed questions about your symptoms and syncope episodes, including whether you have any premonitory symptoms and the circumstances in which your symptoms occur.
Your heart rate and blood pressure will be measured and recorded while you are in different positions including lying down, sitting and standing.
Tests to determine causes of syncope

The head-up tilt test or tilt table test records your blood pressure and heart rate on a minute-by-minute or beat-by-beat basis while the table is tilted in a head-up position at different levels. In some patients, this test may reveal abnormal cardiovascular reflexes that produce syncope.
Blood volume determination: an intravenous (IV) line is inserted into a vein in your arm and a small amount of a radioactive substance (tracer) is injected. Blood samples are then taken and analyzed. The blood volume test is used to evaluate if the amount of blood in your body is appropriate for your gender, height and weight. The blood volume analyzer system used at Cleveland Clinic can provide accurate test results within 35 minutes.
Hemodynamic testing: Three sets of images are taken after a radioactive material has been administered into the IV. The purpose of hemodynamic testing is to evaluate the intravascular pressure and blood flow that occur when the heart muscle contracts and pumps blood throughout the body.
Autonomic reflex testing:A series of different tests are done to monitor blood pressure, blood flow, heart rate, skin temperature and sweating in response to certain stimuli. Taking these measurements can help determine whether or not the autonomic nervous system is functioning normally or if nerve damage has occurred.
Blood volume determination: an intravenous (IV) line is inserted into a vein in your arm and a small amount of a radioactive substance (tracer) is injected. Blood samples are then taken and analyzed. The blood volume test is used to evaluate if the amount of blood in your body is appropriate for your gender, height and weight. The blood volume analyzer system used at Cleveland Clinic can provide accurate test results within 35 minutes.
Hemodynamic testing: Three sets of images are taken after a radioactive material has been administered into the IV. The purpose of hemodynamic testing is to evaluate the intravascular pressure and blood flow that occur when the heart muscle contracts and pumps blood throughout the body.
Autonomic reflex testing:A series of different tests are done to monitor blood pressure, blood flow, heart rate, skin temperature and sweating in response to certain stimuli. Taking these measurements can help determine whether or not the autonomic nervous system is functioning normally or if nerve damage has occurred.
The results of all these tests will help your doctor determine if the cause of your syncope is related to dysfunction of the autonomic nervous system, cardiac dysfunction, neurological disorders or hemodynamic abnormalities.
If necessary after the initial evaluation, other tests may be needed, including electrophysiology studies, autonomic nervous system testing, neurological evaluation, computed tomography scan, Holter monitoring or echocardiogram. Vestibular function testing may be performed to rule out the presence of inner ear problems. If any of these tests are ordered, your doctor will explain why they are needed and what will happen during the test.
Getting the test results
When the test results are available, your referring physician will receive a complete report and treatment recommendations. Your referring physician will explain the results of the test and discuss your treatment options.
How is syncope treated?
Depending on the results of your evaluation and the underlying cause of syncope, treatment is aimed at preventing a syncope recurrence. Treatment may include:
If necessary after the initial evaluation, other tests may be needed, including electrophysiology studies, autonomic nervous system testing, neurological evaluation, computed tomography scan, Holter monitoring or echocardiogram. Vestibular function testing may be performed to rule out the presence of inner ear problems. If any of these tests are ordered, your doctor will explain why they are needed and what will happen during the test.
Getting the test results
When the test results are available, your referring physician will receive a complete report and treatment recommendations. Your referring physician will explain the results of the test and discuss your treatment options.
How is syncope treated?
Depending on the results of your evaluation and the underlying cause of syncope, treatment is aimed at preventing a syncope recurrence. Treatment may include:
Taking new medications or making changes to your current medications
Wearing support garments or compression stockings to improve circulation
Making certain dietary changes such as eating small, more frequent meals; increasing salt, fluid and potassium; and avoiding caffeine and alcohol
Taking certain precautions when changing positions from sitting to standing
Elevating the head of your bed while sleeping. You can do this by using extra pillows or by placing risers under the legs of the head of the bed to elevate it.
Wearing support garments or compression stockings to improve circulation
Making certain dietary changes such as eating small, more frequent meals; increasing salt, fluid and potassium; and avoiding caffeine and alcohol
Taking certain precautions when changing positions from sitting to standing
Elevating the head of your bed while sleeping. You can do this by using extra pillows or by placing risers under the legs of the head of the bed to elevate it.
Avoiding or changing the situations or “triggers” that cause a syncope episode
Pacemaker implantation to regulate the heart rate — only as needed for certain medical conditions
Implantable cardiac defibrillator (ICD), which constantly monitors your heart rate and rhythm and corrects a fast, abnormal rhythm — only as needed for certain medical conditions
Pacemaker implantation to regulate the heart rate — only as needed for certain medical conditions
Implantable cardiac defibrillator (ICD), which constantly monitors your heart rate and rhythm and corrects a fast, abnormal rhythm — only as needed for certain medical conditions
Your health care team will develop a treatment plan that is right for you and your doctor will discuss your treatment options.
Some states require that patients diagnosed with syncope notify the state’s drivers’ license bureau. Check your state’s regulations to be sure.
Outlook
About 30 percent of people with one episode of syncope will have a recurrence. The underlying cause of syncope and the patient’s age, gender and presence of other medical conditions will affect the prognosis or outlook for the future.
With the proper diagnosis and treatment, syncope can be managed and controlled. The prognosis or outlook for the future is dependent on the underlying cause of syncope.
Content Resource: http://www.drugs.com/health-guide/bradycardia.html
Some states require that patients diagnosed with syncope notify the state’s drivers’ license bureau. Check your state’s regulations to be sure.
Outlook
About 30 percent of people with one episode of syncope will have a recurrence. The underlying cause of syncope and the patient’s age, gender and presence of other medical conditions will affect the prognosis or outlook for the future.
With the proper diagnosis and treatment, syncope can be managed and controlled. The prognosis or outlook for the future is dependent on the underlying cause of syncope.
Content Resource: http://www.drugs.com/health-guide/bradycardia.html
Cardiac Specialty Care
• Structural Heart Disease
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• Coronary Intervention
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Peripheral Angioplasty
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Rhythm Management
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
