Angina (an-JI-nuh or AN-juh-nuh) is chest pain or discomfort that occurs if an area of your heart muscle doesn’t get enough oxygen-rich blood. Angina may feel like pressure or squeezing in your chest. The pain also can occur in your shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
Angina isn’t a disease; it’s a symptom of an underlying heart problem. Angina usually is a symptom of coronary heart disease (CHD). CHD is the most common type of heart disease in adults. It occurs if a waxy substance called plaque (plak) builds up on the inner walls of your coronary arteries. These arteries carry oxygen-rich blood to your heart.
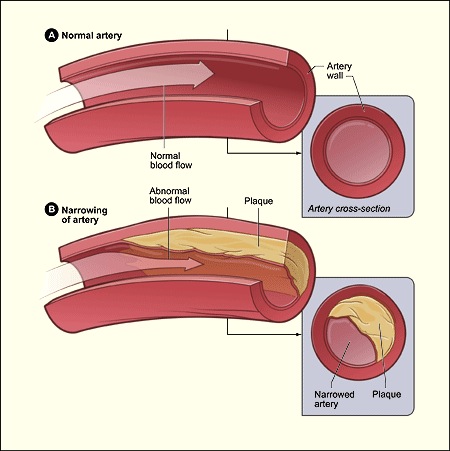
Plaque Buildup in an Artery
Figure A shows a normal artery with normal blood flow. The inset image shows a cross-section of a normal artery. Figure B shows an artery with plaque buildup. The inset image shows a cross-section of an artery with plaque buildup. Plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain. Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
Angina also can be a symptom of coronary microvascular disease (MVD). This is heart disease that affects the heart’s smallest coronary arteries. In coronary MVD, plaque doesn’t create blockages in the arteries like it does in CHD.
Studies have shown that coronary MVD is more likely to affect women than men. Coronary MVD also is called cardiac syndrome X and nonobstructive CHD.
Types of Angina
The major types of angina are stable, unstable, variant (Prinzmetal’s), and microvascular. Knowing how the types differ is important. This is because they have different symptoms and require different treatments.
Stable Angina
Stable angina is the most common type of angina. It occurs when the heart is working harder than usual. Stable angina has a regular pattern. (“Pattern” refers to how often the angina occurs, how severe it is, and what factors trigger it.)
If you have stable angina, you can learn its pattern and predict when the pain will occur. The pain usually goes away a few minutes after you rest or take your angina medicine.
Stable angina isn’t a heart attack, but it suggests that a heart attack is more likely to happen in the future.
Unstable Angina
Unstable angina doesn’t follow a pattern. It may occur more often and be more severe than stable angina. Unstable angina also can occur with or without physical exertion, and rest or medicine may not relieve the pain.
Unstable angina is very dangerous and requires emergency treatment. This type of angina is a sign that a heart attack may happen soon.
Variant (Prinzmetal’s) Angina
Variant angina is rare. A spasm in a coronary artery causes this type of angina. Variant angina usually occurs while you’re at rest, and the pain can be severe. It usually happens between midnight and early morning. Medicine can relieve this type of angina
Angina isn’t a disease; it’s a symptom of an underlying heart problem. Angina usually is a symptom of coronary heart disease (CHD). CHD is the most common type of heart disease in adults. It occurs if a waxy substance called plaque (plak) builds up on the inner walls of your coronary arteries. These arteries carry oxygen-rich blood to your heart.
Plaque Buildup in an Artery
Figure A shows a normal artery with normal blood flow. The inset image shows a cross-section of a normal artery. Figure B shows an artery with plaque buildup. The inset image shows a cross-section of an artery with plaque buildup. Plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain. Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
Angina also can be a symptom of coronary microvascular disease (MVD). This is heart disease that affects the heart’s smallest coronary arteries. In coronary MVD, plaque doesn’t create blockages in the arteries like it does in CHD.
Studies have shown that coronary MVD is more likely to affect women than men. Coronary MVD also is called cardiac syndrome X and nonobstructive CHD.
Types of Angina
The major types of angina are stable, unstable, variant (Prinzmetal’s), and microvascular. Knowing how the types differ is important. This is because they have different symptoms and require different treatments.
Stable Angina
Stable angina is the most common type of angina. It occurs when the heart is working harder than usual. Stable angina has a regular pattern. (“Pattern” refers to how often the angina occurs, how severe it is, and what factors trigger it.)
If you have stable angina, you can learn its pattern and predict when the pain will occur. The pain usually goes away a few minutes after you rest or take your angina medicine.
Stable angina isn’t a heart attack, but it suggests that a heart attack is more likely to happen in the future.
Unstable Angina
Unstable angina doesn’t follow a pattern. It may occur more often and be more severe than stable angina. Unstable angina also can occur with or without physical exertion, and rest or medicine may not relieve the pain.
Unstable angina is very dangerous and requires emergency treatment. This type of angina is a sign that a heart attack may happen soon.
Variant (Prinzmetal’s) Angina
Variant angina is rare. A spasm in a coronary artery causes this type of angina. Variant angina usually occurs while you’re at rest, and the pain can be severe. It usually happens between midnight and early morning. Medicine can relieve this type of angina
Microvascular Angina
Microvascular angina can be more severe and last longer than other types of angina. Medicine may not relieve this type of angina.
Overview
Experts believe that nearly 7 million people in the United States suffer from angina. The condition occurs equally among men and women.
Angina can be a sign of CHD, even if initial tests don’t point to the disease. However, not all chest pain or discomfort is a sign of CHD.
Other conditions also can cause chest pain, such as:
Pulmonary embolism (a blockage in a lung artery)
A lung infection
Aortic dissection (tearing of a major artery)
Aortic stenosis (narrowing of the heart’s aortic valve)
Hypertrophic cardiomyopathy (KAR-de-o-mi-OP-ah-thee; heart muscle disease)
Pericarditis (inflammation in the tissues that surround the heart)
A panic attack
All chest pain should be checked by a doctor.
Content Resource: http://www.nhlbi.nih.gov/health/health-topics/topics/angina/
Microvascular angina can be more severe and last longer than other types of angina. Medicine may not relieve this type of angina.
Overview
Experts believe that nearly 7 million people in the United States suffer from angina. The condition occurs equally among men and women.
Angina can be a sign of CHD, even if initial tests don’t point to the disease. However, not all chest pain or discomfort is a sign of CHD.
Other conditions also can cause chest pain, such as:
Pulmonary embolism (a blockage in a lung artery)
A lung infection
Aortic dissection (tearing of a major artery)
Aortic stenosis (narrowing of the heart’s aortic valve)
Hypertrophic cardiomyopathy (KAR-de-o-mi-OP-ah-thee; heart muscle disease)
Pericarditis (inflammation in the tissues that surround the heart)
A panic attack
All chest pain should be checked by a doctor.
Content Resource: http://www.nhlbi.nih.gov/health/health-topics/topics/angina/
Cardiac Specialty Care
• Structural Heart Disease
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• Coronary Intervention
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Peripheral Angioplasty
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Rhythm Management
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
