Ventricular tachycardia (VT) is a rapid heartbeat that starts in the ventricles.
Causes
Ventricular tachycardia is a pulse rate of more than 100 beats per minute, with at least three irregular heartbeats in a row.
The condition can develop as an early or late complication of a heart attack. It may also occur in patients with:
Cardiomyopathy
Heart failure
Heart surgery
Myocarditis
Valvular heart disease
Ventricular tachycardia can occur without heart disease.
Scar tissue may form in the muscle of the ventricles days, months, or years after a heart attack.
This can lead to ventricular tachycardia.
Ventricular tachycardia can also be caused by:
Anti-arrhythmic medications
Changes in blood chemistry (such as a low potassium level)
Changes in pH (acid-base)
Lack of enough oxygen
“Torsade de pointes” is a form of ventricular tachycardia that is often due to congenital heart disease or the use of certain medications. Symptoms
If the heart rate during a ventricular tachycardia episode is very fast or lasts longer than a few seconds. There may be symptoms such as:
Chest discomfort (angina)
Fainting (syncope)
Light-headedness or dizziness
Sensation of feeling the heart beat (palpitations)
Shortness of breath
Note: Symptoms may start and stop suddenly. In some cases, there are no symptoms.
Exams and Tests
Signs include:
Absent pulse
Loss of consciousness
Normal or low blood pressure
Rapid pulse
Causes
Ventricular tachycardia is a pulse rate of more than 100 beats per minute, with at least three irregular heartbeats in a row.
The condition can develop as an early or late complication of a heart attack. It may also occur in patients with:
Cardiomyopathy
Heart failure
Heart surgery
Myocarditis
Valvular heart disease
Ventricular tachycardia can occur without heart disease.
Scar tissue may form in the muscle of the ventricles days, months, or years after a heart attack.
This can lead to ventricular tachycardia.
Ventricular tachycardia can also be caused by:
Anti-arrhythmic medications
Changes in blood chemistry (such as a low potassium level)
Changes in pH (acid-base)
Lack of enough oxygen
“Torsade de pointes” is a form of ventricular tachycardia that is often due to congenital heart disease or the use of certain medications. Symptoms
If the heart rate during a ventricular tachycardia episode is very fast or lasts longer than a few seconds. There may be symptoms such as:
Chest discomfort (angina)
Fainting (syncope)
Light-headedness or dizziness
Sensation of feeling the heart beat (palpitations)
Shortness of breath
Note: Symptoms may start and stop suddenly. In some cases, there are no symptoms.
Exams and Tests
Signs include:
Absent pulse
Loss of consciousness
Normal or low blood pressure
Rapid pulse
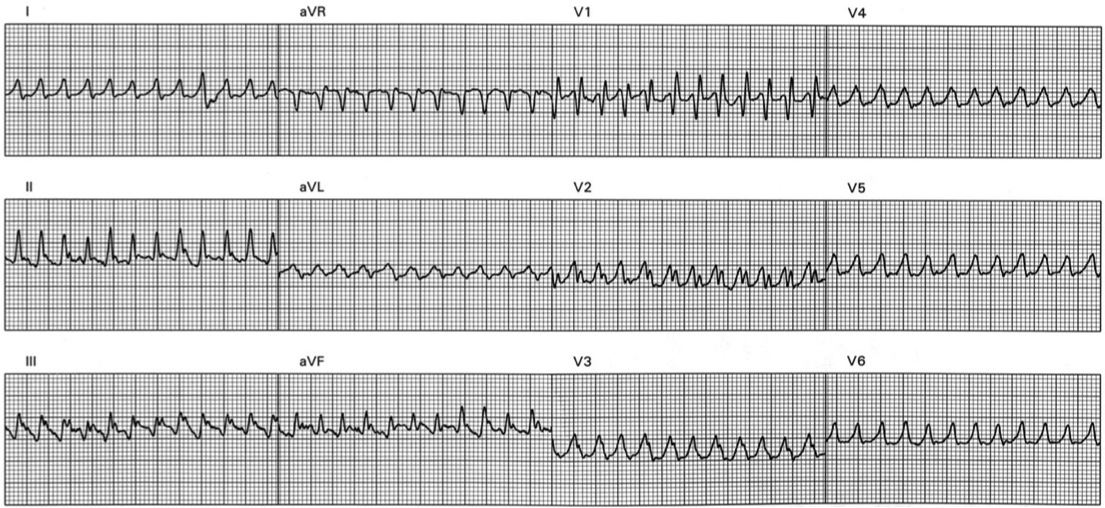
Ventricular tachycardia may be seen on:
Continuous ambulatory electrocardiogram (Holter monitor)
ECG
Intracardiac electrophysiology study (EPS)
Loop recorder
Blood chemistries and other tests may be done.
Treatment
Treatment depends on the symptoms, and the type of heart disorder. Some people may not need treatment.
If ventricular tachycardia becomes an emergency situation, it may require:
CPR
Electrical defibrillation or cardioversion (electric shock)
Anti-arrhythmic medications (such as lidocaine, procainamide, sotalol, or amiodarone) given through a vein
Long-term treatment of ventricular tachycardia may require the use of oral anti-arrhythmic medications (such as procainamide, amiodarone, or sotalol). However, anti-arrhythmic medications may have severe side effects. Their use is decreasing in favor of other treatments.
Some ventricular tachycardias may be treated with an ablation procedure. Radiofrequency catheter ablation can cure certain tachycardias.
A preferred treatment for many chronic (long-term) ventricular tachycardias consists of implanting a device called implantable cardioverter defibrillator (ICD). The ICD is usually implanted in the chest, like a pacemaker. It is connected to the heart with wires.
The doctor programs the ICD to sense when ventricular tachycardia is occurring, and to administer a shock to stop it. The ICD may also be programmed to send a rapid burst of paced beats to interrupt the ventricular tachycardia. You may need to take anti-arrhythmic drugs to prevent repeated firing of the ICD. Outlook (Prognosis)
The outcome depends on the heart condition and symptoms.
Possible Complications
Ventricular tachycardia may not cause symptoms in some people. However, it may be lethal in other people. It is a major cause of sudden cardiac death.
When to Contact a Medical Professional
Go to the emergency room or call the local emergency number (such as 911) if you have a rapid, irregular pulse, faint, or have chest pain. All of these may be signs of ventricular tachycardia.
Prevention
In some cases, the disorder is not preventable. In other cases, it can be prevented by treating heart diseases and correcting blood chemistries.
Content Resource: http://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
Content Resource: http://emedicine.medscape.com/article/159075-overview
Continuous ambulatory electrocardiogram (Holter monitor)
ECG
Intracardiac electrophysiology study (EPS)
Loop recorder
Blood chemistries and other tests may be done.
Treatment
Treatment depends on the symptoms, and the type of heart disorder. Some people may not need treatment.
If ventricular tachycardia becomes an emergency situation, it may require:
CPR
Electrical defibrillation or cardioversion (electric shock)
Anti-arrhythmic medications (such as lidocaine, procainamide, sotalol, or amiodarone) given through a vein
Long-term treatment of ventricular tachycardia may require the use of oral anti-arrhythmic medications (such as procainamide, amiodarone, or sotalol). However, anti-arrhythmic medications may have severe side effects. Their use is decreasing in favor of other treatments.
Some ventricular tachycardias may be treated with an ablation procedure. Radiofrequency catheter ablation can cure certain tachycardias.
A preferred treatment for many chronic (long-term) ventricular tachycardias consists of implanting a device called implantable cardioverter defibrillator (ICD). The ICD is usually implanted in the chest, like a pacemaker. It is connected to the heart with wires.
The doctor programs the ICD to sense when ventricular tachycardia is occurring, and to administer a shock to stop it. The ICD may also be programmed to send a rapid burst of paced beats to interrupt the ventricular tachycardia. You may need to take anti-arrhythmic drugs to prevent repeated firing of the ICD. Outlook (Prognosis)
The outcome depends on the heart condition and symptoms.
Possible Complications
Ventricular tachycardia may not cause symptoms in some people. However, it may be lethal in other people. It is a major cause of sudden cardiac death.
When to Contact a Medical Professional
Go to the emergency room or call the local emergency number (such as 911) if you have a rapid, irregular pulse, faint, or have chest pain. All of these may be signs of ventricular tachycardia.
Prevention
In some cases, the disorder is not preventable. In other cases, it can be prevented by treating heart diseases and correcting blood chemistries.
Content Resource: http://www.nlm.nih.gov/medlineplus/ency/article/000187.htm
Content Resource: http://emedicine.medscape.com/article/159075-overview
Cardiac Specialty Care
• Structural Heart Disease
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• Coronary Intervention
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Peripheral Angioplasty
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Rhythm Management
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
