A pacemaker is a small device that’s placed in the chest or abdomen to help control abnormal heart rhythms. This device uses electrical pulses to prompt the heart to beat at a normal rate.
Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
A heartbeat that’s too fast is called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that’s too slow is called bradycardia (bray-de-KAR-de-ah).
During an arrhythmia, the heart may not be able to pump enough blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or fainting. Severe arrhythmias can damage the body’s vital organs and may even cause loss of consciousness or death.
A pacemaker can relieve some arrhythmia symptoms, such as fatigue and fainting. A pacemaker also can help a person who has abnormal heart rhythms resume a more active lifestyle.
How Does a Pacemaker Work?
A pacemaker consists of a battery, a computerized generator, and wires with sensors at their tips. (The sensors are called electrodes.) The battery powers the generator, and both are surrounded by a thin metal box. The wires connect the generator to the heart.
A pacemaker helps monitor and control your heartbeat. The electrodes detect your heart’s electrical activity and send data through the wires to the computer in the generator.
If your heart rhythm is abnormal, the computer will direct the generator to send electrical pulses to your heart. The pulses travel through the wires to reach your heart.
Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
A heartbeat that’s too fast is called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that’s too slow is called bradycardia (bray-de-KAR-de-ah).
During an arrhythmia, the heart may not be able to pump enough blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or fainting. Severe arrhythmias can damage the body’s vital organs and may even cause loss of consciousness or death.
A pacemaker can relieve some arrhythmia symptoms, such as fatigue and fainting. A pacemaker also can help a person who has abnormal heart rhythms resume a more active lifestyle.
How Does a Pacemaker Work?
A pacemaker consists of a battery, a computerized generator, and wires with sensors at their tips. (The sensors are called electrodes.) The battery powers the generator, and both are surrounded by a thin metal box. The wires connect the generator to the heart.
A pacemaker helps monitor and control your heartbeat. The electrodes detect your heart’s electrical activity and send data through the wires to the computer in the generator.
If your heart rhythm is abnormal, the computer will direct the generator to send electrical pulses to your heart. The pulses travel through the wires to reach your heart.
Newer pacemakers can monitor your blood temperature, breathing, and other factors. They also can adjust your heart rate to changes in your activity.
The pacemaker’s computer also records your heart’s electrical activity and heart rhythm. Your doctor will use these recordings to adjust your pacemaker so it works better for you.
Your doctor can program the pacemaker’s computer with an external device. He or she doesn’t have to use needles or have direct contact with the pacemaker.
Pacemakers have one to three wires that are each placed in different chambers of the heart.
• The wires in a single-chamber pacemaker usually carry pulses from the generator to the right ventricle (the lower right chamber of your heart).
• The wires in a dual-chamber pacemaker carry pulses from the generator to the right atrium (the upper right chamber of your heart) and the right ventricle. The pulses help coordinate the timing of these two chambers’ contractions.
• The wires in a biventricular pacemaker carry pulses from the generator to an atrium and both ventricles. The pulses help coordinate electrical signaling between the two ventricles. This type of pacemaker also is called a cardiac resynchronization therapy (CRT) device.
The pacemaker’s computer also records your heart’s electrical activity and heart rhythm. Your doctor will use these recordings to adjust your pacemaker so it works better for you.
Your doctor can program the pacemaker’s computer with an external device. He or she doesn’t have to use needles or have direct contact with the pacemaker.
Pacemakers have one to three wires that are each placed in different chambers of the heart.
• The wires in a single-chamber pacemaker usually carry pulses from the generator to the right ventricle (the lower right chamber of your heart).
• The wires in a dual-chamber pacemaker carry pulses from the generator to the right atrium (the upper right chamber of your heart) and the right ventricle. The pulses help coordinate the timing of these two chambers’ contractions.
• The wires in a biventricular pacemaker carry pulses from the generator to an atrium and both ventricles. The pulses help coordinate electrical signaling between the two ventricles. This type of pacemaker also is called a cardiac resynchronization therapy (CRT) device.
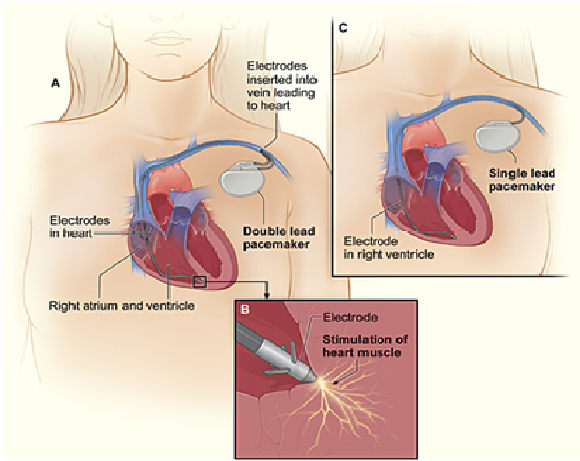
Cross-Section of a Chest with a Pacemaker
The image shows a cross-section of a chest with a pacemaker. Figure A shows the location and general size of a double-lead, or dual-chamber, pacemaker in the upper chest. The wires with electrodes are inserted into the heart’s right atrium and ventricle through a vein in the upper chest. Figure B shows an electrode electrically stimulating the heart muscle. Figure C shows the location and general size of a single-lead, or single-chamber, pacemaker in the upper chest.
Types of Pacemaker Programming
The two main types of programming for pacemakers are demand pacing and rate-responsive pacing.
A demand pacemaker monitors your heart rhythm. It only sends electrical pulses to your heart if your heart is beating too slow or if it misses a beat.
A rate-responsive pacemaker will speed up or slow down your heart rate depending on how active you are. To do this, the device monitors your sinus node rate, breathing, blood temperature, and other factors to determine your activity level.
Your doctor will work with you to decide which type of pacemaker is best for you.
What To Expect During Pacemaker Surgery
Placing a pacemaker requires minor surgery. The surgery usually is done in a hospital or special heart treatment laboratory.
Before the surgery, an intravenous (IV) line will be inserted into one of your veins. You will receive medicine through the IV line to help you relax. The medicine also might make you sleepy.
Your doctor will numb the area where he or she will put the pacemaker so you don’t feel any pain. Your doctor also may give you antibiotics to prevent infection.
First, your doctor will insert a needle into a large vein, usually near the shoulder opposite your dominant hand. Your doctor will then use the needle to thread the pacemaker wires into the vein and to correctly place them in your heart.
An x-ray “movie” of the wires as they pass through your vein and into your heart will help your doctor place them. Once the wires are in place, your doctor will make a small cut into the skin of your chest or abdomen.
He or she will slip the pacemaker’s small metal box through the cut, place it just under your skin, and connect it to the wires that lead to your heart. The box contains the pacemaker’s battery and generator.
Once the pacemaker is in place, your doctor will test it to make sure it works properly. He or she will then sew up the cut. The entire surgery takes a few hours.
What to Expect After Pacemaker Surgery
Expect to stay in the hospital overnight so your health care team can check your heartbeat and make sure your pacemaker is working well. You’ll likely have to arrange for a ride to and from the hospital because your doctor may not want you to drive yourself.
For a few days to weeks after surgery, you may have pain, swelling, or tenderness in the area where your pacemaker was placed. The pain usually is mild; over-the-counter medicines often can relieve it. Talk to your doctor before taking any pain medicines.
Your doctor may ask you to avoid vigorous activities and heavy lifting for about a month after pacemaker surgery. Most people return to their normal activities within a few days of having the surgery.
The image shows a cross-section of a chest with a pacemaker. Figure A shows the location and general size of a double-lead, or dual-chamber, pacemaker in the upper chest. The wires with electrodes are inserted into the heart’s right atrium and ventricle through a vein in the upper chest. Figure B shows an electrode electrically stimulating the heart muscle. Figure C shows the location and general size of a single-lead, or single-chamber, pacemaker in the upper chest.
Types of Pacemaker Programming
The two main types of programming for pacemakers are demand pacing and rate-responsive pacing.
A demand pacemaker monitors your heart rhythm. It only sends electrical pulses to your heart if your heart is beating too slow or if it misses a beat.
A rate-responsive pacemaker will speed up or slow down your heart rate depending on how active you are. To do this, the device monitors your sinus node rate, breathing, blood temperature, and other factors to determine your activity level.
Your doctor will work with you to decide which type of pacemaker is best for you.
What To Expect During Pacemaker Surgery
Placing a pacemaker requires minor surgery. The surgery usually is done in a hospital or special heart treatment laboratory.
Before the surgery, an intravenous (IV) line will be inserted into one of your veins. You will receive medicine through the IV line to help you relax. The medicine also might make you sleepy.
Your doctor will numb the area where he or she will put the pacemaker so you don’t feel any pain. Your doctor also may give you antibiotics to prevent infection.
First, your doctor will insert a needle into a large vein, usually near the shoulder opposite your dominant hand. Your doctor will then use the needle to thread the pacemaker wires into the vein and to correctly place them in your heart.
An x-ray “movie” of the wires as they pass through your vein and into your heart will help your doctor place them. Once the wires are in place, your doctor will make a small cut into the skin of your chest or abdomen.
He or she will slip the pacemaker’s small metal box through the cut, place it just under your skin, and connect it to the wires that lead to your heart. The box contains the pacemaker’s battery and generator.
Once the pacemaker is in place, your doctor will test it to make sure it works properly. He or she will then sew up the cut. The entire surgery takes a few hours.
What to Expect After Pacemaker Surgery
Expect to stay in the hospital overnight so your health care team can check your heartbeat and make sure your pacemaker is working well. You’ll likely have to arrange for a ride to and from the hospital because your doctor may not want you to drive yourself.
For a few days to weeks after surgery, you may have pain, swelling, or tenderness in the area where your pacemaker was placed. The pain usually is mild; over-the-counter medicines often can relieve it. Talk to your doctor before taking any pain medicines.
Your doctor may ask you to avoid vigorous activities and heavy lifting for about a month after pacemaker surgery. Most people return to their normal activities within a few days of having the surgery.
Cardiac Specialty Care
• Structural Heart Disease
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• TAVR
• CardioMEMS (Heart Failure)
• PFO Closure
• Coronary Intervention
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Complex Higher-Risk (And Indicated) Patients (CHIP) Angioplasty
• Atherectomy
• Impella and ECMO Support
• Peripheral Angioplasty
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Varicose Vein Treatment (Venous Ablation)
• DVT thrombectomy - IVC filter
• Carotid Stenting
• Rhythm Management
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
• Pacemaker
• Holter Monitoring
• Exercise Stress Test
• Echocardiography
• Nuclear Stress Test
• Enhanced External Counterpulsation (EECP)
