Coronary Artery Disease (CAD) — also known as Ischemic Heart Disease (IHD) — is a condition where the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked, leading to a reduced blood flow to the heart. This can eventually cause chest pain (angina), heart attacks, heart failure, and arrhythmias. Let’s break this down in detail.
1. Anatomy of the Coronary Arteries
The coronary arteries branch off from the aorta and encircle the heart, supplying it with blood. There are two main coronary arteries:
These arteries feed different parts of the heart muscle.
2. Pathophysiology (What Goes Wrong)
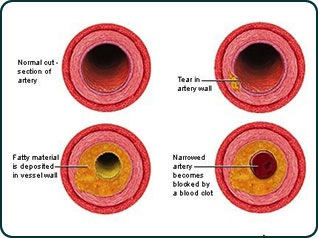
The core issue in CAD is atherosclerosis, a process where plaque (made of cholesterol, fat, calcium, and other substances) builds up on the inner walls of arteries.
Step-by-step progression:
- Endothelial injury (from smoking, high BP, diabetes, etc.)
- Lipid accumulation in the arterial wall.
- Inflammatory response — white blood cells (macrophages) engulf lipids and become foam cells.
- Plaque formation — the vessel wall thickens, narrowing the lumen.
- Plaque rupture can lead to blood clot (thrombus) formation, which can completely block the artery → heart attack.
3. Symptoms of CAD
- Angina pectoris (chest pain) — often triggered by exertion or stress.
- Shortness of breath
- Fatigue
- Heart palpitations
- Silent ischemia — no symptoms, common in diabetics.
- If complete blockage occurs: Myocardial Infarction (heart attack)
???? 4. Diagnosis of CAD
- Electrocardiogram (ECG) – looks for ischemic changes.
- Stress test – monitors heart function during exertion.
- Echocardiogram – checks heart muscle and valve function.
- Coronary angiography – gold standard; uses contrast dye and X-rays to visualize blockages.
- CT coronary angiogram – less invasive scan for detecting plaque.
???? 5. Risk Factors
Modifiable:
- Smoking
- High blood pressure (hypertension)
- High cholesterol (especially LDL)
- Diabetes
- Obesity
- Physical inactivity
- Unhealthy diet
- Stress
Non-modifiable:
- Age
- Gender (males more at risk earlier)
- Family history
???? 6. Treatment of CAD
A. Lifestyle Changes
- Quit smoking
- Heart-healthy diet (low in saturated fats, more fruits/veggies)
- Regular exercise
- Weight loss
- Stress management
B. Medications
- Statins – lower cholesterol
- Aspirin – reduces clot formation
- Beta-blockers – reduce heart’s workload
- ACE inhibitors – lower BP and protect heart
- Nitrates – relieve angina
- Calcium channel blockers
C. Procedures & Surgery
- Angioplasty + Stenting: A catheter is used to open up a narrowed artery, and a stent is placed to keep it open.
- Coronary Artery Bypass Grafting (CABG): Healthy vessels from the leg or chest are used to bypass blocked arteries.
???? 6. Treatment of CAD
A. Lifestyle Changes
- Quit smoking
- Heart-healthy diet (low in saturated fats, more fruits/veggies)
- Regular exercise
- Weight loss
- Stress management
B. Medications
- Statins – lower cholesterol
- Aspirin – reduces clot formation
- Beta-blockers – reduce heart’s workload
- ACE inhibitors – lower BP and protect heart
- Nitrates – relieve angina
- Calcium channel blockers
C. Procedures & Surgery
- Angioplasty + Stenting: A catheter is used to open up a narrowed artery, and a stent is placed to keep it open.
- Coronary Artery Bypass Grafting (CABG): Healthy vessels from the leg or chest are used to bypass blocked arteries.

